CHOLERA
Cholera, a waterborne disease caused by the bacterium Vibrio cholerae, has plagued humanity for centuries, causing widespread illness and death. Understanding the historical context, epidemiology, clinical presentation, treatment, and prevention measures of cholera is crucial to addressing its outbreaks. This essay delves into these aspects, providing a comprehensive overview of cholera and its impact on public health.
Historical Context
Cholera has a long and storied history, with the first recorded pandemic occurring in 1817. Since then, there have been seven cholera pandemics, with the most recent beginning in 1961 and continuing today. The first six pandemics, originating in India, spread globally, causing millions of deaths. The seventh pandemic, caused by the El Tor biotype of Vibrio cholerae, started in Indonesia and has spread to various parts of the world, particularly affecting developing countries with inadequate water and sanitation infrastructure.
Epidemiology
Cholera is primarily spread through contaminated water and food. The disease thrives in areas with poor sanitation, inadequate water treatment, and overcrowded living conditions. Seasonal patterns are often observed, with outbreaks occurring more frequently during the rainy season in endemic areas.
Global Burden
Cholera remains a significant public health challenge in many parts of the world. According to the World Health Organization (WHO), there are an estimated 1.3 to 4 million cases of cholera each year, resulting in 21,000 to 143,000 deaths. The highest burden is seen in sub-Saharan Africa, South Asia, and parts of Latin America and the Caribbean.
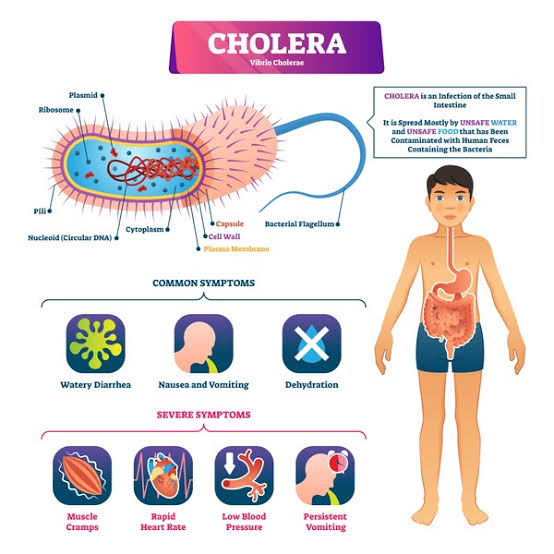
Pathophysiology
Vibrio cholerae produces a potent enterotoxin, cholera toxin, which is responsible for the severe diarrhea characteristic of the disease. The toxin disrupts the normal absorption and secretion processes in the intestines, leading to a massive loss of fluids and electrolytes. This rapid dehydration can be fatal if not promptly treated.
Clinical Presentation
Cholera has a wide spectrum of clinical manifestations, ranging from asymptomatic infections to severe, life-threatening dehydration. The incubation period is typically 2-3 days but can range from a few hours to 5 days.
Symptoms
- Mild Cases: These may present with mild diarrhea and abdominal cramps, often indistinguishable from other common diarrheal illnesses.
- Moderate to Severe Cases: These are characterized by sudden onset of profuse, watery diarrhea (often described as “rice-water stools”), vomiting, and rapid dehydration. Patients may exhibit signs of severe dehydration, including sunken eyes, dry mouth, decreased skin turgor, and lethargy. Severe cases can lead to hypovolemic shock and death within hours if not treated.
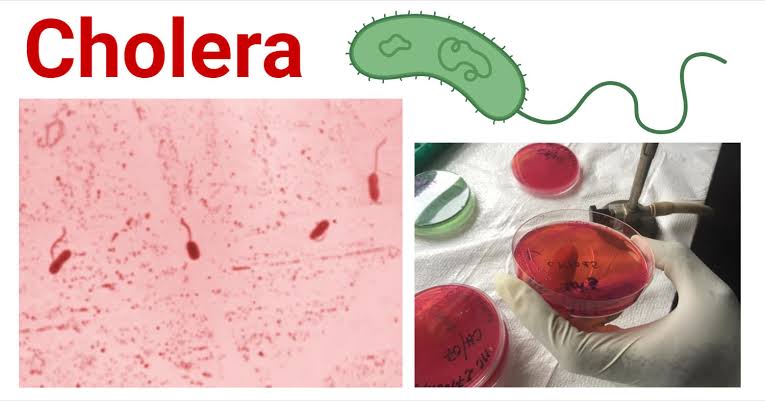
Diagnosis
Diagnosis of cholera is primarily clinical in areas with known outbreaks. Laboratory confirmation is achieved by isolating Vibrio cholerae from stool samples using culture techniques or rapid diagnostic tests (RDTs). RDTs provide results within minutes and are particularly useful in resource-limited settings.
Treatment
The cornerstone of cholera treatment is rapid rehydration to replace lost fluids and electrolytes. Antibiotic therapy can also play a role, particularly in severe cases.
Rehydration
- Oral Rehydration Therapy (ORT): ORT is the first-line treatment for most cholera patients. Oral rehydration salts (ORS) solution, containing a balanced mixture of glucose and electrolytes, is administered to prevent and treat dehydration.
- Intravenous Rehydration: In cases of severe dehydration, where patients are unable to drink sufficient ORS or are in shock, intravenous (IV) fluids are necessary. Ringer’s lactate is the preferred IV fluid due to its balanced electrolyte composition.
Antibiotics
Antibiotics can reduce the duration and volume of diarrhea, but they are not a substitute for rehydration therapy. Commonly used antibiotics include doxycycline, azithromycin, and ciprofloxacin. Antibiotic resistance is an emerging concern, necessitating ongoing surveillance and stewardship.
Prevention and Control
Preventing cholera involves a multifaceted approach, including improving water, sanitation, and hygiene (WASH), as well as vaccination.
Water, Sanitation, and Hygiene (WASH)
- Safe Water Supply: Ensuring access to clean drinking water is paramount. This can be achieved through various methods, including chlorination, filtration, and safe storage practices.
- Sanitation: Proper disposal of human waste and the use of latrines can significantly reduce the contamination of water sources.
- Hygiene: Promoting handwashing with soap, especially before eating and after using the toilet, is crucial in preventing the spread of cholera.
Vaccination
Oral cholera vaccines (OCVs) are an effective tool in preventing cholera outbreaks. There are currently two WHO-prequalified OCVs: Dukoral and Shanchol. Vaccination campaigns are particularly important in endemic areas and during outbreaks to provide immediate protection.
Case Study: The Haiti Cholera Outbreak
One of the most notable recent cholera outbreaks occurred in Haiti following the devastating earthquake in 2010. The outbreak, which began in October 2010, resulted in over 800,000 cases and nearly 10,000 deaths. The introduction of cholera to Haiti was linked to a United Nations peacekeeping camp, highlighting the importance of monitoring and controlling potential sources of infection.
Response Efforts
The response to the Haitian cholera outbreak involved a combination of emergency medical interventions, including the establishment of cholera treatment centers, mass distribution of ORS and water purification tablets, and a large-scale vaccination campaign. Despite these efforts, the outbreak underscored the challenges of responding to cholera in a resource-limited setting and the need for sustained investments in water and sanitation infrastructure.
Cholera Outbreak in June
Cholera, a highly contagious bacterial disease caused by Vibrio cholerae, continues to pose significant public health challenges globally, particularly in regions with inadequate water and sanitation infrastructure. The onset of the rainy season in many parts of the world, often in June, can exacerbate the conditions that lead to cholera outbreaks. This essay examines the factors contributing to cholera outbreaks in June, the epidemiological patterns observed, and the response strategies employed to control and prevent the spread of the disease.

Seasonal Patterns and Contributing Factors
Cholera outbreaks are often influenced by environmental and climatic conditions. The rainy season, which typically begins in June in many cholera-endemic regions, creates an environment conducive to the spread of Vibrio cholerae. The following factors contribute to the heightened risk of cholera outbreaks during this period:
- Water Contamination: Heavy rains can lead to the contamination of drinking water sources with fecal matter containing Vibrio cholerae. Flooding can overwhelm sanitation systems, leading to the spread of the bacteria.
- Poor Sanitation and Hygiene: Inadequate sanitation facilities and poor hygiene practices become even more problematic during the rainy season. Overflowing latrines and open defecation can increase the risk of waterborne diseases.
- Increased Mobility: Seasonal migrations for agricultural work or other reasons can lead to the spread of cholera from endemic areas to new regions, facilitating outbreaks.
- Warm Temperatures: Warmer temperatures during the rainy season can promote the growth and survival of Vibrio cholerae in aquatic environments.
Epidemiological Patterns
Historical data and epidemiological studies indicate that cholera outbreaks often surge in June and continue throughout the rainy season. The following patterns are commonly observed:
- Rapid Increase in Cases: Cholera cases can increase rapidly during the early weeks of the rainy season, necessitating swift public health responses.
- Geographic Spread: Outbreaks often start in coastal or riverine areas and spread to inland regions as contaminated water moves through waterways.
- Demographic Impact: Vulnerable populations, including children, the elderly, and those with compromised immune systems, are disproportionately affected by cholera outbreaks.
Response Strategies
Effective management of cholera outbreaks during the rainy season requires a multifaceted approach, involving rapid medical intervention, public health measures, and community engagement. Key response strategies include:
Rapid Medical Response
- Treatment Centers: Establishing cholera treatment centers in affected areas ensures that patients receive prompt and appropriate care. These centers are equipped with oral rehydration salts (ORS), intravenous fluids, and antibiotics.
- Surveillance and Reporting: Enhanced disease surveillance and reporting systems help in the early detection of outbreaks and the monitoring of case numbers.
Water, Sanitation, and Hygiene (WASH) Interventions
- Safe Water Supply: Providing access to clean drinking water is crucial. This can involve distributing water purification tablets, setting up chlorination points, and ensuring the safe storage of water.
- Sanitation Facilities: Improving sanitation facilities, such as building latrines and ensuring proper waste disposal, can reduce the contamination of water sources.
- Hygiene Promotion: Educating communities about the importance of handwashing with soap, safe food handling, and other hygiene practices is essential in preventing the spread of cholera.
Vaccination Campaigns
- Oral Cholera Vaccines (OCVs): Mass vaccination campaigns using OCVs can provide immediate protection to at-risk populations. These campaigns are particularly effective in areas with ongoing or imminent outbreaks.
- Targeted Vaccination: Vaccination efforts can be targeted to high-risk groups, such as those living in flood-prone areas or regions with poor sanitation infrastructure.
Case Study: Recent Outbreaks
To illustrate the challenges and responses to cholera outbreaks in June, consider the following recent examples:
Bangladesh (June 2023)
In June 2023, heavy monsoon rains in Bangladesh led to widespread flooding and a subsequent cholera outbreak in the Cox’s Bazar district. The influx of refugees from neighboring Myanmar, combined with overcrowded living conditions and inadequate sanitation, exacerbated the situation.
- Response: The Bangladesh Ministry of Health, with support from international organizations, launched a large-scale vaccination campaign, reaching over 500,000 people. Mobile treatment units were deployed to provide medical care in hard-to-reach areas. Efforts to improve water and sanitation facilities in refugee camps were also intensified.
Yemen (June 2022)
Yemen has experienced repeated cholera outbreaks due to ongoing conflict, poor sanitation, and a collapsing healthcare system. In June 2022, heavy rains and flooding triggered a new wave of cholera cases, particularly in the Al Hudaydah and Taiz governorates.
- Response: The World Health Organization (WHO) and local health authorities established cholera treatment centers and distributed ORS and water purification tablets. Public health campaigns focused on educating communities about hygiene practices and safe water use. Despite these efforts, the ongoing conflict posed significant challenges to the response.
Challenges and Future Directions
Addressing cholera outbreaks during the rainy season involves overcoming several challenges:
- Resource Limitations: Many affected regions lack the necessary resources for effective outbreak response, including medical supplies, trained healthcare workers, and infrastructure.
- Access and Security: In conflict-affected areas, access to affected populations can be restricted, and security concerns can hinder response efforts.
- Climate Change: Increasingly unpredictable weather patterns and more severe rainfall events due to climate change may lead to more frequent and intense cholera outbreaks.
Innovative Approaches
To enhance the effectiveness of cholera outbreak response during the rainy season, innovative approaches are being explored:
- Early Warning Systems: Integrating climate data with health surveillance systems can help predict and prepare for cholera outbreaks before they occur.
- Community-Based Approaches: Empowering communities to take an active role in cholera prevention, including the management of water sources and hygiene promotion, can lead to more sustainable outcomes.
- Mobile Health Technologies: Utilizing mobile technology for real-time data collection, disease reporting, and public health messaging can improve the speed and efficiency of response efforts.
Conclusion
Cholera remains a formidable public health challenge, particularly in resource-limited settings. Effective management of cholera outbreaks requires a combination of rapid medical intervention, robust public health infrastructure, and preventive measures such as improved water and sanitation. Vaccination campaigns and innovative approaches offer promising avenues for reducing the burden of cholera. However, sustained efforts and global cooperation are essential to achieve long-term control and eventual eradication of this devastating disease.


